What you are about to read is an opportunity for every EMS leader from around the country, and the world, to connect with their law enforcement colleagues and work together towards safe and consistent methods of treatment that will no doubt reduce the amount of deaths in custody.
9News in Denver, Colorado spent a year in search of an answer to a question: Why do people continue to die underneath the elbows, knees and bodies of officers?
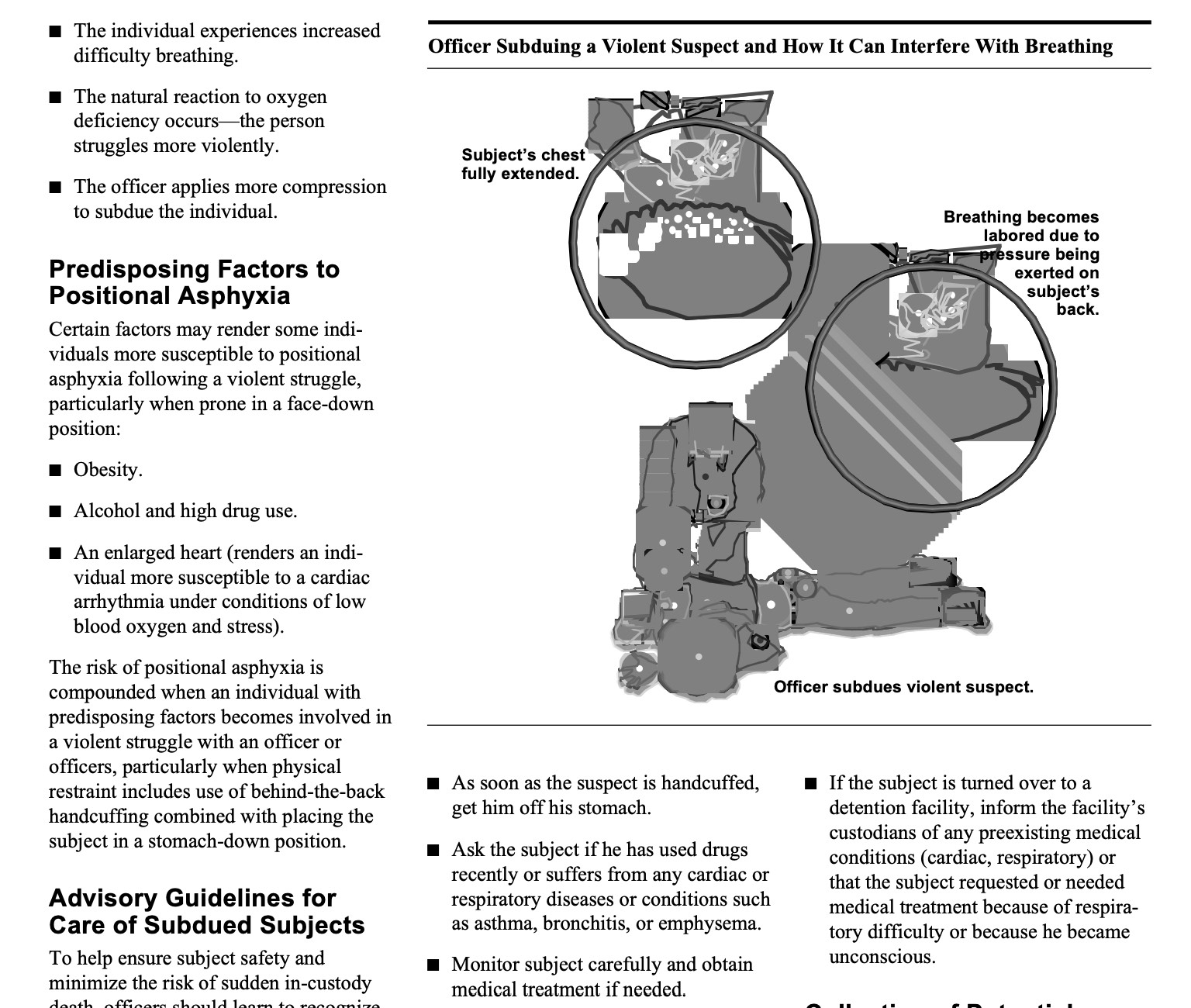
As the above video discusses, nearly 50% of deaths in custody had some type of mental health complaint. Regardless of the etiology of someone's delirium (head injury, mental health crisis, drug induced rage, or even low blood sugar) we need to ensure law enforcement recognizes the need to get someone off their stomach as quickly as possible. Law enforcement also needs to assume that resisting against restraints could mean a medical emergency and involve educated EMS providers sooner than later.
Avoid the death position: Get them off their stomach as soon as possible to prevent positional asphyxiation.
Leaders have an opportunity to work together to ensure safe policies and clinical protocols are in place and practiced. The proper use of medications (such as benzodiazepines, haldol, Ketamine) and equipment (EtCO2 monitoring, backboards, restraints) are critical to ensure a patient in extremis does not continue to build up lactic acid that will precipitate a cardiac arrest.
Cell phones, live streaming, & body camera footage
Objective video recordings have revealed horrific deaths and racially motivated murders that make it hard to deny the realities of racial injustice and discrimination beyond a few "bad actors."
The body camera footage of paramedics called to help Earl Moore Jr, December 18, 2022, show two EMS providers in Springfield, Illinois blatantly disregarding human life.
It becomes more and more apparent that there are systemic issues related to the training police officers or paramedics receive - or said more accurately the lack of training.
Is this a new issue?
Nearly 30 years ago the U.S. Department of Justice issued a bulletin (June 1995) based on a report from the International Association of Chiefs of Police to help raise awareness of this dangerous issue.
Major portions of this bulletin are drawn from a report prepared by the International Association of Chiefs of Police for the National Institute of Justice (NIJ), based on research conducted by Dr. Charles S. Petty, Professor of Forensic Pathology, University of Texas, and Dr. Edward T.McDonough, Deputy Chief Medical Examiner, State of Connecticut, and reviewed by the Less-Than-Lethal Liability Task Group.
Research has shown for years that the face down prone position and prone restraints will cause respiratory compromise and death.
What the research has been telling us about "the death position"
Abstract: “Introduction: The physiology of many sudden, unexpected arrest-related deaths (ARDs) proximate to restraint has not been elucidated. A sudden decrease in central venous return during restraint procedures could be physiologically detrimental. The impact of body position and applied weight force on central venous return has not been previously studied. In this study, we use ultrasound to measure the size of the inferior vena cava (IVC) as a surrogate of central venous return in the standing position, prone position, and with weight force applied to the thorax in the prone position…. Conclusions: The physiology involved in many sudden, unexpected ARDs has not been elucidated. However, in our study, we found a significant decrease in IVC diameter with weight force compression to the upper thorax when the subject was in the prone position. This may have implications for the tactics of restraint to aid in the prevention of sudden, unexpected ARD cases.”
Abstract: “Background: The prone maximal restraint (PMR) position has been used by law enforcement and emergency care personnel to restrain acutely combative or agitated individual. The position places the subject prone with wrists handcuffed behind the back and secured to the ankles. Prior work has indicated a reduction in inferior vena cava (IVC) diameter associated with this position when weight force is applied to the back. It is therefore possible that this position can negatively impact hemodynamic stability. Objectives: We sought to measure the impact of PMR with and without weight force on measures of cardiac function including vital signs, oxygenation, stroke volume (SV), IVC diameter, cardiac output (CO) and cardiac index (CI). Conclusions: PMR with and without weight force did not result in any changes in CO or other evidence of cardiovascular or hemodynamic compromise.”
Abstract: “The study sought to determine the physiologic effects of the prone maximum restraint (PMR) position in obese subjects after intense exercise. We designed an experimental, randomized, cross-over trial in human subjects conducted at a university exercise physiology laboratory. Ten otherwise healthy, obese (BMI > 30) subjects performed a period of heavy exertion on a cycling ergometer to 85 percent of maximum heart rate, and then were placed in one of three positions in random order for 15 min: (1) seated with hands behind the back, (2) prone with arms to the sides, (3) PMR position. While in each position, mean arterial blood pressure (MAP), heart rate (HR), minute ventilation (VE), oxygen saturation (SaO2), and end tidal CO2 (etCO2) were measured every 5 min. There were no significant differences identified between the three positions in MAP, HR, VE, or O2s at at any time period. There was a slight increase in heart rate at 15 min in the PMR position over the prone position (95 vs. 87). There was a decrease in end tidal CO2 at 15 min in the PMR over the prone position (32 mmHg vs. 35 mmHg). In addition, there was no evidence of hypoxia or hypoventilation during any of the monitored 15 min position periods. Conclusion: In this small study of obese subjects, there were no clinically significant differences in the cardiovascular and respiratory measures comparing seated, prone, and PMR position following exertion.”
Have We Seen Any Changes?
While there are many organizations who are problem aware, they might not all be solution aware.
Progressive policing leaders, EMS departments and medical directors have worked together to educate other systems on safe patient restraint. Yet deaths in police custody continue to happen across the nearly 16,000 police departments in the US, employing just under 1M full time officers according to census.gov.
This article published in the FBI's law enforcement bulletin is written for law enforcement by a police chief and EMS medical director who clearly outline a proven approach for safe restraint while in custody. This approach has been practiced for over 20 years and allows paramedics to evaluate, assess, and intervene to ensure patient and crew safety.
“Public safety personnel must be caring and compassionate and demonstrate concern when interacting with unruly individuals or those with mental illness.”
Police Practice:
Safe Restraint of Agitated Patients
By James J. Gerace and Michael W. Dailey, M.D.
“Using a medical backboard to restrain agitated persons … is the best practice to reduce negative in-custody patient outcomes, allow medical evaluation, assure safe monitoring and patient transfers to the hospital, and minimize staff injuries.”
Steps Leaders Can Take
- Proactively engage with colleagues in law enforcement leadership.
Ensure police departments and EMS departments work together towards a common goal of patient and provider safety.
Share the above article that highlights best practices and proven methods. - Let's question our firmly held beliefs of how things have always been.
Discussing the problems is one step, talking about solutions and taking action towards an ideal future is a productive step. - Let's listen to others.
Listen to learn more from various stakeholders so that we can understand and empathize with those that we serve and those that work within our organizations.
In the wake of multiple high profile killings
NASEMSO issued a Statement of Unity & Equity in 2020, calling on our industry leaders, "We must identify any biases within ourselves, and have the courage and empathy to fully commit our platform and resources to create an inclusive, diverse society with the cornerstone of equality for all."
What we are doing about it?
In 2020, the EMS Leadership Academy hosted a series of conversations to address racism and unconscious bias. Since then over 900 participants enrolled in this free training series.
In 2023, thanks to a grant provided to the Southern Tier Healthcare System (STEMS) of Olean, New York, the EMS Leadership Academy teamed up with renowned safety expert, Dr. I. David Daniels of ID2 Solutions, to take a new training approach to Diversity, Equity, Inclusion & Justice.
Leading With Empathy: A Three Stepped Approach to Fostering More Diversity, Equity, Inclusion & Justice - Designed for Care Providers
This introduction discusses how to help foster diversity, equity, inclusion, justice, and belonging in caregiver organizations. Strategies for problem-solving and success are highlighted, such as maintaining a learner's mindset, understanding internal systems and environments, and fostering non-judgmental conversations. Reticular activating systems and the amygdala are discussed in order to create conscious awareness and prevent blind spots. Additionally, the importance of leadership, transformational education, and understanding different psychological processes is discussed. Strategies for creating a meaningful and sustainable world are discussed to ensure all people are treated with respect and understanding.
This section provides an overview of the importance of psychological safety for care providers. It explains the differences between safety as a condition and feeling safe as a subjective emotion. Research on employee engagement is discussed, with three levels of psychological safety identified (physical, cognitive, and emotional). The potential risks posed by systems and roles that are not well-defined or that may have an adverse impact on certain populations are examined. Finally, solutions are suggested for organizations to prioritize creating a shared belief system and encouraging diversity, equity, fairness, and justice in order to mitigate these risks.

This last section emphasizes the importance of considering mental and psychosocial health when creating change. Five key takeaways are discussed in detail such as starting from scratch, following the clues, being mindful of structure, being creative, and striving for a safe and accepting environment. Additionally, communication, cooperation, appreciative inquiry, and creating sustainable outcomes are highlighted as tools to create the desired outcome and relationships. Additionally, creative problem-solving, honest feedback and building diverse and inclusive environments need to be addressed in order to be successful.